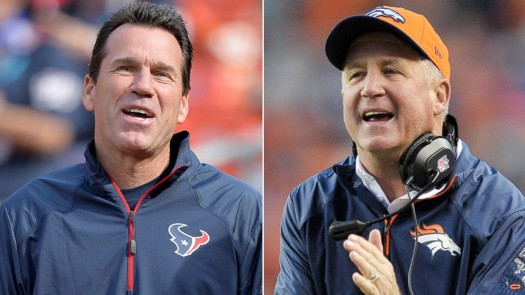
First, NFL coach for the Denver Broncos, John Fox, falls ill on the golf course and is undergoing open-heart surgery two days later. Then, NFL coach for the Tenessee Titans, Gary Kubiak, drops to his knees walking to the locker room at halftime of a nationally televised game, suffering what is later diagnosed as a mini-stroke. Having TWO NFL coaches suffer heart related medical emergencies over the course of the weekend really reinforces the importance of doing everything we can to keep our hearts healthy. Let’s take a deeper look at what happened to the coaches, and what you can do to help fend off these scary conditions…
Coach Fox’s Aortic Valve Replacement
Let’s start with Coach Fox, who found out he needed an aortic valve replacement surgery. Coach Fox was advised by doctors months ago that his defective aortic valve would require this procedure following the 2013 season. Fox was taken to a hospital in the Charlotte area a couple days later when he started feeling light-headed while playing golf. Fox did not suffer a heart attack but underwent a battery of tests that revealed the need for immediate aortic valve replacement surgery.
What is an Aortic Valve Replacement?
Aortic valve replacement is a surgery done for aortic valve stenosis (think “narrowing”) and aortic valve regurgitation (think “leaking”). Ever heard of those conditions? Here’s what they entail…
Aortic valve stenosis is a narrowing of the aortic valve . The aortic valve allows blood to flow from the heart’s lower left chamber (ventricle) into the aorta and to the body. Stenosis prevents the valve from opening properly, forcing the heart to work harder to pump blood through the valve. This causes pressure to build up in the left ventricle and thickens the heart muscle. Your heart can make up for aortic valve stenosis and the extra pressure for a long time. But at some point, it won’t be able to keep up the extra effort of pumping blood through the narrowed valve. This can lead to heart failure.
Aortic valve regurgitation is a problem with the aortic valve. The aortic valve allows blood to flow from the heart’s lower left chamber (ventricle) into the aorta and to the body. When the heart rests between beats, the valve closes to keep blood from flowing backward into the heart. When you have aortic valve regurgitation, the aortic valve doesn’t close as it should. With each heartbeat, some of the blood leaks back (regurgitates) through the aortic valve into the left ventricle. The body does not get enough blood, so the heart has to work harder to make up for it.
What are the Symptoms?
Many patients have no symptoms whatsoever, even when the stenosis (narrowing) or insufficiency (leak) are severe. That said, symptoms may include:
• Fatigue
• Get tired easily
• Loss of energy
• Swelling of the ankles
• Palpitations (extra or skipped heart beats)
• Enlargement of the aorta because of high blood pressure or hardening of the arteries.
• Endocarditis (an infection in the heart)
• Shortness of breath
• Chest pain/pressure
• Dizziness or loss of consciousness
What are the Risk Factors?
Certain medical problems or conditions make it more likely that you will develop an aortic valve stenosis and/or regurgitation:
• Calcium buildup – Aging can cause calcium buildup around the aortic valve, which can make the normally thin and flexible valve flaps thick and stiff. This is also called calcific aortic valve stenosis. Many of the things that increase the risk of atherosclerosis and heart disease are the same for aortic valve stenosis. They include smoking, high cholesterol, high blood pressure, diabetes, and being male.
• Birth defect – Sometimes a person is born with a bicuspid aortic valve that has two flaps instead of the normal three. Over time, the valve becomes damaged and calcium builds up. As the valve narrows, less blood can flow through it.
• Infection – Rheumatic fever can cause scar tissue to build up at the edges of the valve. Rheumatic fever is not common now. But if you had it as a child, you may have an increased risk.
• Artificial valve – Aortic valve diseases also may develop in an artificial aortic valve that is made from human or animal tissue.
• Kidney failure
• Smoking
How is it diagnosed?
The diagnosis is made after your physician reviews your symptoms, performs a physical exam and listens for a murmur, and evaluates the results of your diagnostic tests.
What Happens During Aortic Valve Replacement Surgery?
In an aortic valve replacement surgery, the damaged valve is removed and replaced with an artificial valve (mechanical or tissue). If you are going to have valve replacement surgery, your doctor may suggest that you have a coronary angiogram/catheterization test. This test can show if you have blockages in your coronary arteries (as part of coronary artery disease). If you have serious blockages, your doctor may want to do a coronary artery bypass surgery at the same time as the valve replacement surgery.
Could aortic valve replacement surgery be right for me?
According to American College of Cardiology (ACC)/American Heart Association (AHA) guidelines, candidates for aortic valve replacement include the following patients:
• Symptomatic patients with severe aortic stenosis
• Patients with severe aortic stenosis undergoing coronary artery bypass surgery
• Patients with severe aortic stenosis undergoing surgery on the aorta or other heart valves
• Patients with severe aortic stenosis and LV systolic dysfunction
Coach Kubiak’s Mini-Stroke (aka TIA)
Coach Kubiak, 52, suffered a transient ischemic attack (TIA), a condition that causes stroke symptoms by temporarily stopping blood flow to the brain.
What is a transient ischemic attack (TIA)?
Some people call a TIA a “mini-stroke,” because the symptoms are like those of a stroke but don’t last long. A TIA happens when blood flow to part of the brain is blocked or reduced, often by a blood clot. After a short time, blood flows again and the symptoms go away. With a stroke, the blood flow stays blocked, and the brain has permanent damage.
A TIA is a warning: it means you are likely to have a stroke in the future. If you think you are having a TIA, call 911. Early treatment can help prevent a stroke. If you think you have had a TIA but your symptoms have gone away, you still need to call your doctor right away.
What are the symptoms?
Symptoms of a TIA are the same as symptoms of a stroke. But symptoms of a TIA occur suddenly and don’t last very long. Most of the time, they go away in 10 to 20 minutes. They may include:
• Sudden numbness, tingling, weakness, or paralysis in your face, arm, or leg, especially on only one side of your body.
• Sudden vision changes.
• Sudden trouble speaking.
• Sudden confusion or trouble understanding simple statements.
• Sudden problems with walking or balance.
• A sudden, severe headache that is different from past headaches.
What Causes a TIA?
A blood clot is the most common cause of a TIA. Blood clots can be the result of hardening of the arteries (atherosclerosis), heart attack, or abnormal heart rhythms. Brain cells are affected within seconds of the blockage. That causes symptoms in the parts of the body controlled by those cells. After the clot dissolves, blood flow returns, and the symptoms go away. Sometimes a TIA is caused by a sharp drop in blood pressure that reduces blood flow to the brain. This is called a “low-flow” TIA and it’s not as common as other types.
What are the Risk Factors?
In general, you are more at risk for TIA if:
• You smoke
• You have high blood pressure
• Your cholesterol level is higher than average
• You have diabetes
• You are overweight
• You don’t exercise on a regular basis
• You drink large amounts of alcohol
What can I do to Help Prevent TIA?
• Treat any health problems you have.
• Manage high blood pressure or high cholesterol by working with your doctor.
• Manage diabetes. Keep your blood sugar levels within a target range.
• If your doctor advises you to take aspirin or a blood thinner, take it. This can help prevent a stroke.
• Take your medicine exactly as prescribed. Call your doctor if you think you are having a problem with your medicine.
• Adopt a healthy lifestyle.
• Don’t smoke or allow others to smoke around you.
• Limit alcohol to 2 drinks a day for men and 1 drink a day for women.
• Stay at a healthy weight. Being overweight makes it more likely you will develop high blood pressure, heart problems, and diabetes. These conditions make a stroke more likely.
• Do activities that raise your heart rate. Get at least 30 minutes of exercise on most days of the week. Walking is a good choice. You also may want to do other activities, such as running, swimming, cycling, or playing tennis or team sports.
How is TIA Treated?
If you’ve had a TIA, you may need further testing and treatment after you’ve been checked by your doctor. If you have a high risk of stroke, you may have to stay in the hospital for treatment.
Your treatment for a TIA may include taking medicines to prevent a stroke or having surgery to reopen narrow arteries. Medicines may include aspirin, clopidogrel, dipyridamole with aspirin, or warfarin. If your carotid arteries are significantly blocked, you may need surgery to reopen the narrowed arteries (carotid endarterectomy).
Source:
http://www.latimes.com/sports/football/nfl/la-sp-kubiak-fox-20131106,0,226525.story#axzz2jsn00iPt
http://emedicine.medscape.com/article/150638-overview
http://www.webmd.com/stroke/tc/transient-ischemic-attack-tia-topic-overview